In the first wave of digital health, AI was a “back-office” engine. Why would we say so? AI back then just silently processed data to help providers with billing or triage. But as we move through 2026, we have entered the era of digital patient engagement 2.0.
We’ve spent a lot of time thinking about why the healthcare industry’s push toward “patient-centricity” often feels like it’s hitting a glass ceiling.
Yes, in this digital era, we have the portals, the wearables, and the automated pings, yet we are still chasing the same ghost: sustained behavioral change.
All healthtech leaders can agree that data is the fuel, but you’re also realizing that data without context is just noise to a patient.
That’s what makes the transition to digital patient engagement 2.0 so critical for those of us leading healthtech organizations today.
It’s a shift from just providing access to providing agency.
When a patient receives a health recommendation they don’t understand, or a notification that feels like it’s coming from a “black box,” the intent gets lost.
That’s where the friction starts.
And in health, friction doesn’t just mean a dropped user—it means a missed treatment or a worsening condition.
Key insights
Here are the strategic takeaways for leaders moving toward patient engagement 2.0:
-
From access to agency: Engagement 2.0 pivots from passive portals to proactive, transparent clinical loops.
-
Trust as a metric: Use XAI (via $SHAP$ or $LIME$) to turn “black box” nudges into actionable patient logic.
-
Behavioral ROI: Transparency reduces alert fatigue and increases long-term treatment adherence.
-
Infrastructure over algorithms: Solving EHR data silos and the “accuracy vs. interpretability” paradox is the prerequisite for 2.0 success.
What is digital patient engagement 2.0?
If version 1.0 was about the “digitization of the health record’s paper trail” (think PDFs in portals, appointment reminders, and basic telehealth) then digital patient engagement 2.0 is about the intelligence of the interaction.
It’s a move away from passive tracking and toward proactive, personalized loops.
In 2.0, engagement isn’t measured by how many times a patient logs in; it’s measured by how well the technology facilitates a “collaborative intelligence” between the patient, the AI, and the clinical team.
It’s defined by these 3 core shifts:
- From transactional to relational: We aren’t just sending reminders; we’re building a narrative. The system understands the patient’s lifestyle context—their sleep, their stress, their location—and adapts its voice accordingly.
- From insights to actionable logic: It’s no longer enough to show a graph of blood glucose levels. Engagement 2.0 explains why the spike happened and what the next three hours should look like to correct it.
- From “black box” to transparency: This is the most vital piece. In 2.0, the “how” and “why” behind an AI’s suggestion are visible. We’ve realized that for a patient to take a high-stakes health action, they need to trust the logic, not just the brand.
Ultimately, 2.0 is about moving the needle from “compliance” (doing what you’re told) to “concordance” (doing what you understand).
When the support is designed to be transparent and human, confidence changes, and behavior follows.
What are the healthcare leaders’ takes on digital patient engagement 2.0
We’ve been tracking how the top minds in the field are framing this evolution.
The consensus is clear: if 1.0 was about the “what,” 2.0 is entirely about the “how” and the “why.”

The ROI of informed action in patient engagement
The business case for 2.0 is no longer theoretical. Experts are moving away from “soft” engagement metrics toward hard clinical outcomes.
According to research cited by McKinsey (2025) and Health Affairs, patients who are actively involved in shared decision-making — a cornerstone of 2.0 — showed 5.3% lower overall medical costs and 12.5% fewer hospital admissions.
Our takeaway: Digital patient engagement 2.0 isn’t just a “nice to have” for patient satisfaction; it’s a financial imperative for value-based care models.
The rise of agentic literacy
In their 2026 Global Healthcare Outlook, Deloitte highlights that over 50% of health system executives are now pivoting their investments toward “Agentic AI” – the AI that doesn’t just chat, but acts and explains.
Mytonomy’s 2026 Guide adds that the “literacy gap” is the new frontier. They argue that patient engagement 2.0 requires “microlearning”—streaming bite-sized, video-based explanations directly to a patient’s device at the exact moment of a clinical trigger.
Our takeaway: We are moving from “prescribing medicine” to “prescribing education” that is as easy to consume as a Netflix stream.
Moving from “monitoring” to “partnership”
At HIMSS 2026, the narrative has shifted toward supporting clinical judgment.
Experts from Wolters Kluwer emphasize that digital patient engagement 2.0 is about trusted AI.
They argue that the bottleneck isn’t the data—it’s the validation of that data. For a patient to stay engaged, the AI must deliver a “clinically validated medication intelligence layer” that explains the logic behind a nudge.
5 ways explainable AI (XAI) drives digital patient engagement 2.0
When we talk about digital patient engagement 2.0, we’re really talking about a shift in the power dynamic.
In the old world, the AI was a “black box” that handed down edicts. In the new world, the AI is a collaborator.
But for that collaboration to work, the patient needs to understand the “logic” of the machine.
That’s where Explainable AI (XAI) moves from a technical luxury to a core business requirement.
Here are the 5 ways we’re seeing XAI actually move the needle on patient behavior and clinical outcomes.
1. Moving from “blind compliance” to “trust calibration”
We’ve all seen the data: patients stop using digital health tools because they don’t trust a notification they can’t verify. XAI solves this by providing local explanations.
Instead of a generic nudge saying, “Time to take your insulin,” an XAI-driven system says: “Your glucose is trending 15% higher than your usual Tuesday average after lunch. We recommend your dose now to prevent a 4 PM crash.”
2. Feature attribution: identifying the “why” behind the medical alert
Patients are often overwhelmed by “lifestyle noise.” They don’t know if their heart rate is up because of stress, lack of sleep, or a genuine cardiac event.
Engineers use $SHAP$ (SHapley Additive exPlanations) values to determine which features are driving a model’s prediction.
In patient engagement 2.0, we surface these “weights” to the patient in plain English:
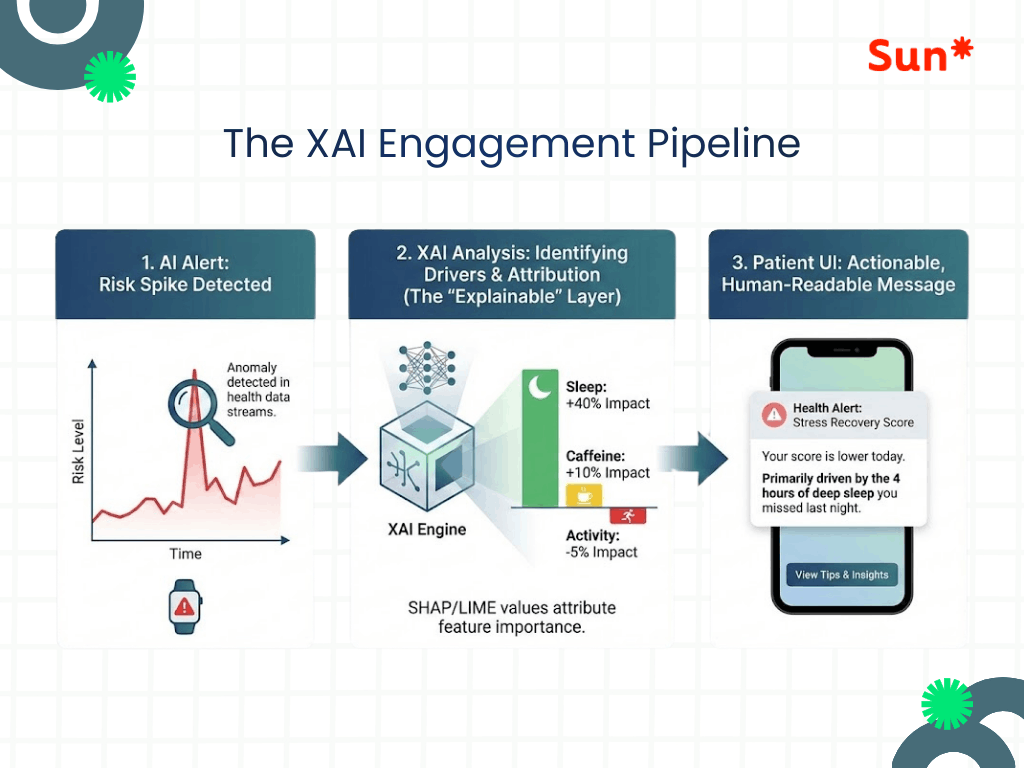
3. Reducing alert fatigue through precision
One of the biggest engagement killers is the “cry wolf” effect. If a wearable pings a patient ten times for a false positive, they’ll delete the app by the eleventh.
XAI allows us to create a verification loop.
By explaining the evidence behind an alert (e.g., “This arrhythmia alert was triggered by a specific pattern in your $ECG$ data that deviates from your baseline”), we increase the “signal-to-noise” ratio.
When patients know why an alert is high-priority, their response rate stays high over the long term.
4. Algorithmic fairness and bias mitigation
As leaders, one of our biggest “keep-me-up-at-night” risks is algorithmic bias.
If our engagement engine works better for one demographic than another, we aren’t just failing our patients — we’re facing a massive regulatory and ethical liability.
XAI serves as our internal audit log.
By using techniques like $LIME$ (Local Interpretable Model-agnostic Explanations), our teams can see if an AI is over-weighting certain demographic markers incorrectly.
5. Bridging the patient-provider gap
The biggest bottleneck in 2.0 is often the 15-minute doctor’s visit. A patient walks in with 3 months of “black box” data, and the doctor doesn’t have time to parse it.
XAI creates a common language.
It provides a summary that both the patient and the doctor can understand: “The AI suggested a change in medication because it observed a persistent correlation between your salt intake and blood pressure spikes on weekends.”
This turns the data from a “tech problem” into a “clinical conversation,” driving higher satisfaction for both parties.
Our lessons: 4 technical bottlenecks we’ve solved in the move to digital patient engagement 2.0
This is the part of the conversation where we have to be honest about the “messy middle.”
We all want the transparency of XAI, but as a healthcare IT outsourcing partner who has sat in the room while engineers and clinical leads debate the roadmap, we know there are specific patterns where these initiatives often stall.
1. The “interpretability vs. accuracy” paradox
This is the classic engineering tug-of-war.
The most powerful models — like Deep Learning and Neural Networks — are notoriously “black boxes.” They provide incredible predictive accuracy but are nearly impossible to explain.
- The bottleneck: Teams often find that to make a model “explainable” for a patient, they have to use simpler, less accurate models (like Decision Trees).
- Our solution: Instead of dumbing down the model, we wrap the complex AI in an interpretability layer (using $SHAP$ or $LIME$) that “translates” the complex math into a narrative for the patient.
It’s more computationally expensive, but it’s the only way to keep the accuracy without losing trust.
2. The EHR silo and data latency
You can’t explain a patient’s health trajectory if you’re only looking at 10% of their data.
- The bottleneck: Most engagement tools live on a “data island.” They see the steps from a Fitbit but don’t see the labs from the Epic or Cerner EHR.
Without that clinical context, your XAI “explanation” is often incomplete or, worse, medically misleading. - Our solution: The bottleneck isn’t the AI—it’s the FHIR (Fast Healthcare Interoperability Resources) integration.
Until the data flows in real-time between the clinical record and the patient app, “Engagement 2.0” stays in a perpetual pilot phase.
3. The translation gap: data science vs. health literacy
We’ve seen brilliant engineering teams build XAI dashboards that are technically perfect but, practically, not so useful.
- The bottleneck: An engineer sees a $SHAP$ value of $+0.85$ and thinks “success.” A patient sees that and feels overwhelmed.
- Our solution: We often fail to account for cognitive load. If we give a patient a data science lecture every time they get a notification, they will experience “explanation fatigue” and tune out.
The bottleneck here is UI/UX design services they had — taking complex attribution data and turning it into a single, human sentence that a 70-year-old with Type 2 diabetes can act on instantly.
4. The validation loop
In patient engagement 1.0, a “bug” in an app was an annoyance.
In 2.0, where AI is giving clinical explanations, a bug is a safety risk.
- The bottleneck: Every time your AI “explains” something to a patient, that explanation is technically a clinical claim.
- Our solution: Regulatory bodies (like the FDA under 2026 SaMD guidelines) are increasingly looking at not just the output of the AI, but the explanation itself. Companies are hitting a bottleneck where their QA and clinical validation cycles are doubling because they have to verify that the AI’s “reasoning” is medically sound across every possible patient edge case.
Call out to leaders
The transition to digital patient engagement 2.0 isn’t a “flip the switch” moment. It’s an iterative process of building trust through transparency.
The leaders who win won’t just have the best algorithms; they’ll have the most understandable ones.
We have to stop asking, “How do we get more data?” and start asking, “How do we make the data we have mean something to the person holding the phone?”
By architecting for explainability, we move the AI from an oracle that must be obeyed to a partner that can be understood.
Let’s build the bridge together!
Moving from “black box” AI to a transparent 2.0 ecosystem is a massive technical and cultural lift. Our team has done +50 projects in helping healthtech organizations bridge this gap — navigating the technical bottlenecks of XAI while keeping the patient experience human-centric.
If you’re ready to move beyond passive monitoring and start building a high-trust, high-engagement platform, let’s talk.