Updated: January 2026
The healthcare landscape in 2026 has reached a definitive crossroads. As a leader in the healthtech field, you’ve likely realized this isn’t the time to simply “watch” the market. It’s a time for high-stakes decisions.
If you’ve been tracking the usual news cycles, you’ve seen the noise: telehealth pivots, blockchain integration, or the next generation of wearables. But through our work on dozens of healthcare IT outsourcing projects, we’ve observed one shift that carries more strategic weight than the rest: AI in clinical decision-making.
From our viewpoint, this isn’t just another feature to add to your roadmap. It represents a fundamental restructuring of how we, as an industry, diagnose and treat: a shift toward cognitive augmentation powered by medical foundation models.
We’ve noticed a clear pattern in the healthtech businesses we partner with: if you’re still debating whether to integrate AI-powered clinical support, the window of opportunity is narrowing.
We believe the question for 2026 has shifted from if you should adopt AI, to how seamlessly you can weave it into your core operations.
The stakes feel existential because the advantages are compounding. In our experience, startups that successfully bridge the gap between “code” and “clinical workflow” today see massive gains in accuracy and patient outcomes. Those who hesitate don’t just fall behind; they risk losing the relevance they worked so hard to build.
In this article, we want to share our observations on why clinical AI has emerged as the most decisive trend for 2026. We’ll look at the critical decisions this technology forces upon your organization and the failure patterns we’ve seen leaders encounter.
The window for a strategic lead is still open, but based on what we’re seeing in development cycles right now, the time to gear up is today.
Key Takeaways – Clinical AI in 2026
- Strategic Priority: AI in clinical decision-making is the #1 tech trend for 2026, shifting from a “feature” to a foundational requirement for survival.
- Primary Bottleneck: The “velocity gap,” aka the delay between having a vision and achieving operational scale, is the leading cause of startup failure.
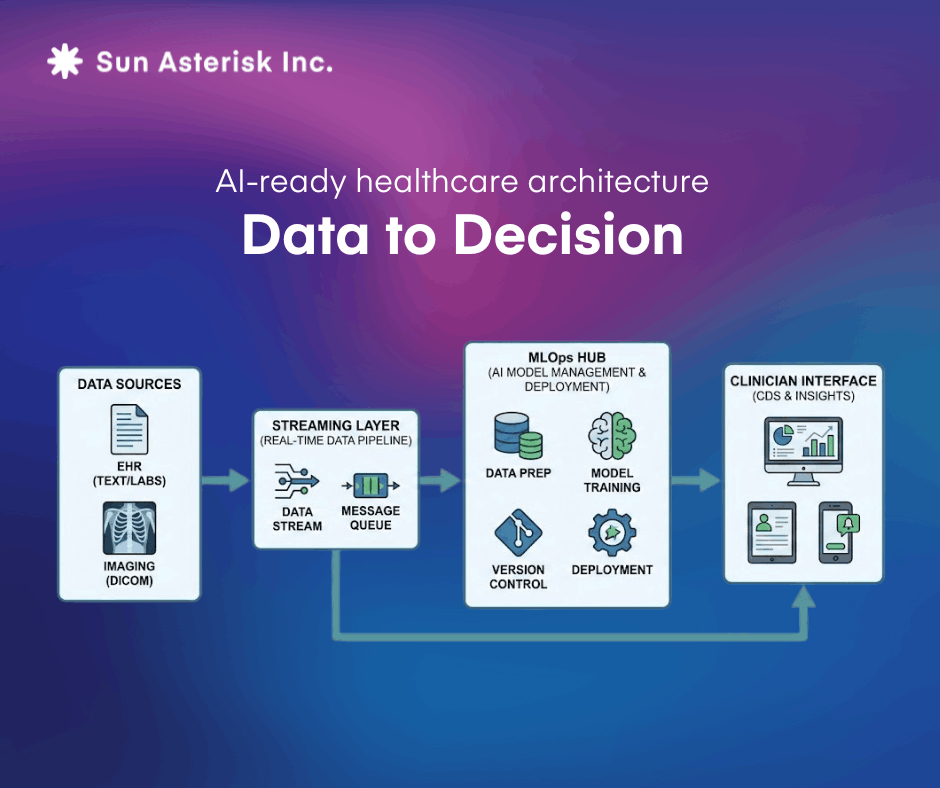
- Architecture Shift: Successful integration requires moving from legacy, EMR-centric silos to real-time, FHIR-integrated data mesh architectures.
- Human Factor: 80% of AI success depends on workflow redesign and clinician trust, rather than the algorithm itself.
Why is AI in clinical decision-making the dominant healthcare trend for 2026?
The numbers alone tell a compelling story. The global health AI market, which is valued at $11 billion in 2021, is projected to explode to $187 billion by 2030, representing a compound annual growth rate exceeding 35%.
But as we often discuss with our partners and clients, the “why” matters more than the “how much.”
The real story in 2026 isn’t just growth, but it’s the shift from experimental tools to clinical must-haves.
1. Step-function changes, not marginal gains
In the early days of healthtech, we were happy with 5% efficiency gains. Today, the data we’re seeing suggests we’ve moved into “step-function” territory.
Consider the impact:
- Radiology: Studies in The Lancet Oncology have shown AI-supported screenings detecting 20% more cancers while nearly halving the workload for clinicians.
- Predictive Care: We’ve seen projects where machine learning models predict unplanned hospital readmissions with enough accuracy to trigger interventions before the patient even feels a symptom.
When you’re building a startup, these aren’t just “features.” They are fundamental shifts in clinical capability that redefine what your product can actually do for a hospital’s bottom line.
2. The “master enabler” effect
We like to think of AI in clinical decision-making as a “foundational” layer.
If you get this right, everything else in your stack becomes more valuable. Remote monitoring stops being a data dump and starts being a high-accuracy predictive risk stratification engine.
- Telehealth becomes more than a video call; it becomes an AI-powered triage system.
- Remote monitoring stops being a data dump and starts being a “deterioration early-warning system.”
- Personalized medicine finally has the engine it needs to synthesize genomic data and real-time biometrics into something a doctor can actually use.
In our experience, startups that treat AI as a core platform find it much easier to innovate. Those who treat it as a “plugin” often find themselves hitting technical ceilings when they try to scale.
3. Your 12–18 month window
The “wait and see” era is over. Unlike previous tech waves (like EHRs) that took a decade to settle, the AI cycle is moving at a breakneck pace.
Working in the AI healthtech projects, we’ve actually been surprised by just how rapidly the volume of AI-driven initiatives is increasing. What was a niche conversation two years ago has become the default starting point for almost every new project we touch.
What we’ve observed is the emergence of “data moats.” The startups moving decisively right now are:
- Building proprietary datasets that late-movers won’t be able to buy
- Cementing regulatory pathways that create a high barrier to entry
- Warping clinical workflows around their tools, making them “sticky” and hard to replace
As Dr. Luqman Lawal (Mayo Clinic Platform) recently noted, reckless speed can be a trap, but strategic speed is essential. You need to gear up your “healthcare engine” now, because the world moves to the next AI stage faster than most roadmaps can handle.
By now, your 2026 strategic roadmap is likely already in motion. But as we’ve seen time and again, execution is where the visionary meets the reality.
Looking back at the clinical AI builds we navigated throughout 2025, we’ve noticed that the most promising roadmaps often snag on the same recurring hurdles. We’ve distilled these observations into specific “operational killers” – the kind of invisible friction points that look perfectly fine on a slide deck but can derail a startup the moment you hit scale.
We want to share these insights to help you stress-test your current plan against the actual real-life challenges we’ve encountered, ensuring your “2026 engine” is as resilient as it is innovative 👉 2026 Clinical AI Execution Audit: Operational Killers to Avoid
4. Beyond digitization: it’s about augmenting our mindset and workflows
If the last decade was about digitization (moving paper to screens), 2026 is about cognitive augmentation. This is a critical distinction for your leadership team.
Previous waves didn’t really change how a doctor thought; they just changed where they wrote. AI-driven decision support changes the cognitive process itself.
💡 Our observation: Leaders who treat this as a simple “IT project” almost always struggle.
Those who see it as an organizational transformation – focusing on Explainable AI (XAI) and algorithmic transparency – are the ones we see riding above the adoption wave.
The question isn’t whether AI will reshape clinical decision-making. That transformation is already underway.
The question is which organizations will lead it and which will spend the next decade struggling to catch up.
The Decision Architecture: What 2026 Will Make You Choose
True story we’ve seen along the way of our custom healthtech software development services: the most successful leaders aren’t just “implementing AI” but making a series of interconnected, high-stakes bets.
In this landscape, mistakes are expensive to reverse.
Here are the three pivotal decision points that will define your healthcare strategy this year.
1. Should healthtech startups build or partner for their clinical AI infrastructure?
The “buy” option is increasingly a commodity in 2026; if everyone can buy the same API, where is your moat? We’re seeing businesses struggle with the “build vs. partner” trilemma:
- The build trap: Building in-house offers total control, but it consumes your most precious resource: time. Unless your AI is your primary IP, we’ve seen startups bleed runway trying to build infrastructure that they could have partnered for.
- The strategic partnership: This has become the “middle path” for the agile. We’ve noticed that combining your clinical domain expertise with an external AI-native partner allows you to move at a 2x pace. As the World Economic Forum has highlighted, resilient healthcare systems in 2026 are being built on these “hybrid” foundations.
2. How does data architecture create a competitive moat for clinical AI?
You’ll be surprised by how many teams still treat data as a “storage” problem rather than a “competitive” one. In 2026, your data architecture determines your speed of iteration.
- Centralized vs. federated: Do you go for a unified repository (high power, high privacy risk) or a federated approach (lower risk, higher technical complexity)?
- The quality must-have: Regardless of the “where,” the “what” is non-negotiable. We’ve seen dozens of AI initiatives stall because the data was “dirty”, inconsistent coding, and unstructured fields. Our takeaway? Invest in your data engine and your AI logic simultaneously. Building AI on poor data is an expensive way to fail.
Whether you choose centralized vs. federated, your FHIR API integration strategy is non-negotiable. We are seeing a massive shift toward Data Mesh in healthcare to handle the volume of 2026 workloads.
3. Why do AI implementations fail without clinical workflow redesign?
This is the most common point of friction we encounter. There is a persistent misconception that AI can be “added” to a workflow like a plugin.
- The reality: Effective clinical AI shifts the entire diagnostic sequence. It moves decision points earlier in the patient journey.
- You must choose to either proactively redesign the workflow with clinicians at the table, or accept that your tool will be ignored by the front line. There is no middle ground in 2026. “Half-hearted” integration produces systems that look great in a demo but fail in the ward.
4. The talent & budget shift
In 2026, AI isn’t an “incremental” budget line but a reallocation of your core IT spending.
- The 20% rule: The startups gaining real traction are moving 15-25% of their total IT budget toward AI capabilities. This often means making the tough call to defund legacy maintenance or “nice-to-have” features.
- The talent hybrid (or what we’d like to call “fluid workforce”): Since the “AI talent war” is only intensifying, we recommend a hybrid strategy: hire your strategic leads internally, but use healthcare IT outsourcing partners to scale the “heavy lifting” of development.
The meta-decision tech leaders can make today
Finally, the most important observation we can share is this: indecision is the only fatal move. In 2026, the landscape shifts in weeks, not quarters.
In 2026, healthtech leaders who maintain a strategic lead are those who recognize that an “imperfect” action today is often more valuable than a “perfect” analysis six months from now.
In our experience, the greatest risk isn’t making a wrong decision; it’s treating every decision like a “one-way” door. This leads to organizational paralysis while the market and your competitors move on to the next AI stage.
Whether you’re weighing a new data architecture or preparing for a complex clinical integration, we can help you navigate the “one-way doors” with the confidence of someone who has been there before.
The Technical Backbone: Moving from EMR-Centric to AI-Ready
As shared above, if there is one thing we’ve learned from the healthcare IT builds of 2025, it’s this: AI is not a “plug-and-play” feature. It is a fundamental shift in how your infrastructure breathes.
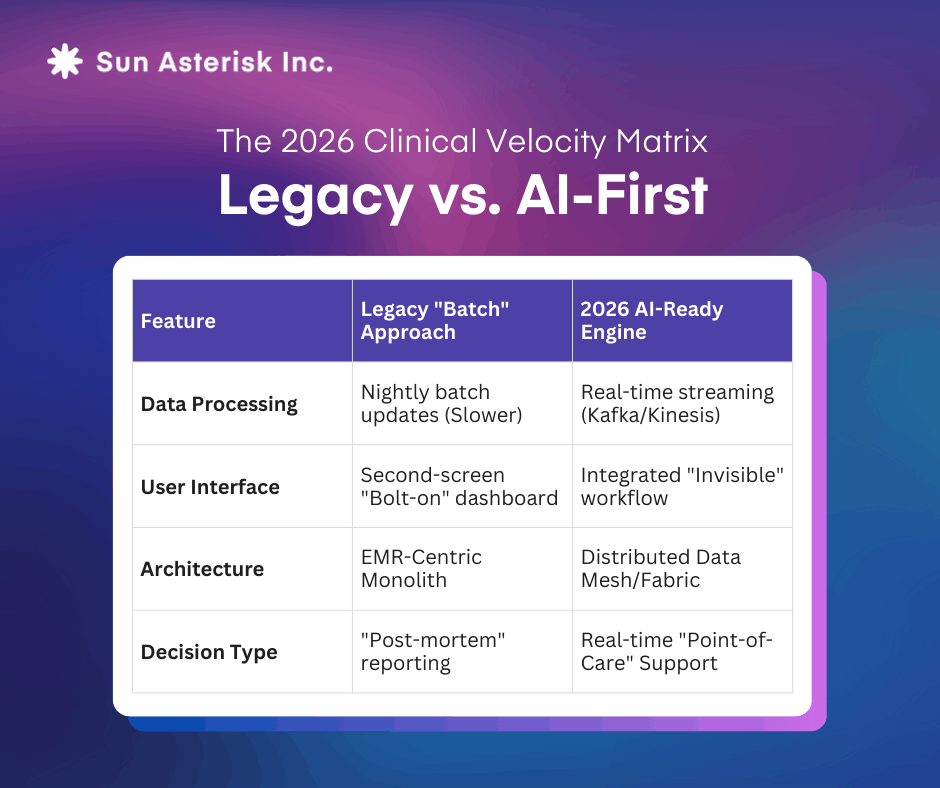
Startups that try to “bolt” AI onto a legacy EMR-centric architecture hit a performance wall almost immediately. To help you evaluate your current stack, here are the architectural shifts we’re seeing define the market in 2026.
1. Breaking the EMR monolith
Data flows into the EMR, sits within the EMR, and gets extracted from the EMR for reporting. This model worked adequately for documentation and basic analytics, but fails catastrophically for AI clinical applications.
For decades, the EMR was the sun around which all healthcare data orbited. But for AI, the EMR is often too slow and too siloed to be the primary hub.
- The shift: We’re helping teams move toward a data fabric approach where the EMR remains the system of record, but AI platforms hold the topical authority for clinical insight.
- The goal: You need real-time data pipelines that can ingest structured fields, medical imaging, and device feeds simultaneously. If your AI has to wait for an EMR export to “think,” it’s already too late.
2. The performance gap: batch vs. real-time
Legacy healthcare runs on “batch” processing, and reports are generated overnight. But you well know that clinical decision support lives in the milliseconds.
- Our observation: Take sepsis prediction. Identifying a risk 12 hours early only saves lives if that insight reaches the clinician’s screen in seconds.
- Reality: Real-life demands real-time data pipelines (like Kafka or Kinesis). In our recent projects, we’ve found that the “velocity gap” between a batch-processed model and a real-time one is often the difference between a tool that is a “nice-to-have” and one that is essential infrastructure.
3. Edge computing: AI at the point of care
We’ve noticed a growing need for “Edge AI”- executing models locally in the ER or ICU rather than the cloud.
- Why it matters: In high-stakes environments, you can’t afford a network hiccup or unacceptable latency.
- Your decision: You have to decide which parts of your roadmap require “Edge” resilience and which can stay in the cloud. Over-engineering the edge adds massive complexity, but ignoring it makes your system brittle in a crisis.
4. MLOps: the scaling anchor
We’ve been surprised by how many teams overlook model governance. Without robust MLOps infrastructure, you’ll eventually lose track of which model version is running where, or why a model’s performance is “drifting” over time.
- Our recommendation: Treat MLOps for healthcare (versioning, data lineage, and model drift monitoring) as a core part of your build, not an afterthought. In 2026, an ungoverned model is a massive regulatory and clinical liability.
5. The integration “tax”
The most consistent failure pattern we’ve observed? Underestimating the integration tax. The AI model itself is usually only 20% of the work. The other 80% is the “grunt work” of integrating with:
- Existing EMR workflows (via FHIR APIs)
- Secure clinical messaging systems
- Identity management and audit logs
Our takeaway for 2026: A mediocre AI model on a brilliant, integrated architecture will almost always outperform a “perfect” model that sits in an isolated silo.
Reconfiguring Your Team for 2026
If your 2026 digital roadmap is the “what,” your organization is the “how.”
However, the technical “heavy lifting” is only half the battle. The other half is building a team structure that doesn’t reject the AI like a foreign body.
The new stakeholders in your technical team
We’ve noticed that the traditional IT hierarchy is being replaced by “AI-native” roles. For example, in an agile startup, you might not hire four new people, but your current team needs to absorb these specific functions:
- The clinical translator: We’ve seen that projects move 40% faster when there’s a Clinical Informaticist bridging the gap between data science and the ward. They ensure the AI solves a real doctor’s problem, not just a data scientist’s curiosity.
- MLOps engineers: These are the “pit crew” for your AI. They ensure your models don’t “drift” or lose accuracy as 2026’s messy real-world data flows in.
- Ethicists & bias auditors: This is no longer optional. Concrete data shows that algorithmic bias is a major hurdle; for example, a 2019 study published in Science found that an algorithm used on more than 200 million people was significantly less likely to refer Black patients to specialized programs compared to white patients with the same level of need.
In 2026, we think that the most successful teams are those that prioritize responsible AI and perform bias mitigation early to avoid regulatory fallout.
The 80/20 rule of budgeting
One of our biggest “lessons learnt from the field” is the budget mismatch.
- The pattern: Many startups allocate 80% of their budget to tech and 20% to training.
- Our conclusion: We’ve seen this lead to pilot fails. The organizations that successfully scale are those that invert this ratio over time. They realize that clinical behavior change is the actual “product” they are selling.
Breaking the silos with “dual-track” structures
Healthcare is notoriously siloed, but AI demands a cross-functional strike team.
- What we recommend: Instead of occasional “check-in” meetings between your devs and clinicians, we’ve seen success with a dual-track organization. You keep your operational core stable while building a separate, highly agile AI unit that has the authority to move fast and break (and fix) workflows in real-time.
Cultural shift: from intuition to augmentation
This is the deepest challenge. We’ve been surprised by how much clinical intuition is guarded as a professional identity.
We don’t frame AI as a replacement. We frame it like a modern stethoscope. It’s a tool that amplifies what the clinician is already good at. When you involve skeptics early in the design phase, we’ve noticed the “resistance” turns into “refinement.”
The Final Check: Is Your Organization Ready to Lead?
As we look at the landscape in January 2026, the tech is ready. The question is: is your organization ready to catch it?
We’ve spent the last year observing the “invisible” reasons why some healthtech plans soar while others stall. Most often, it’s not the code — it’s the governance, the bias checks, and the workflow integration that make the difference.